Treatment of patella dislocation:
when does MPFL plastic surgery help?
A kneecap sprain is a sudden, very uncomfortable and painful condition that usually develops after playing sports or sudden movements. When the kneecap (patella) slips sideways from the socket of the femur, it can cause not only severe pain but also permanent instability. Repetitive dislocation can lead to long-term damage to cartilage surfaces and premature wear. We will show when conservative therapy is enough and when surgical stabilisation of the patella may be an option, summarising the essentials and benefits of MPFL surgery (MPFLplasty).
Why does the kneecap pop out? - The most common causes of kneecap sprains
The kneecap (patella) normally moves in the groove in front of the femur, while the hamstring muscle tenses. However, in some cases it can move sideways and even jump out of place - this is called a kneecap sprain. The phenomenon is not only painful, but can also be frightening, especially if it is the first time it has occurred.
One-off sprain or recurring problem?
The first sprain is often caused by a sudden, wrong movement or a sports accident. The ligaments that stabilise the kneecap laterally (MPFL = medial patellofemoral ligament) may be stretched or damaged, but in many cases full recovery can be achieved with proper rest, bracing and physiotherapy.
If, however, the kneecap slips out of place several times, it recurrent patellar tendonitis we can talk. This means that the ligaments can no longer hold the patella in the correct position and the kneecap becomes unstable, which can lead to further dislocations, cartilage and tissue damage. In this case, conservative treatments are no longer sufficient and surgical stabilisation of the kneecap becomes necessary, for example MPFL plastics.

Dr. Péter Doszkocs
Orthopaedic traumatologist, hip and knee surgeon, lower limb specialist, robotic surgeon
Online booking:
Budafoki Road surgery: Thursday
Bokor street surgery: Week of the other days
Please choose the service that suits you
The control fee is valid for 3 months after the initial examination, for the same complaint.
- 1. Select the service you need from the drop-down box!
- 2. Use the calendar to choose a date that suits you!
- 3. Enter your details to register or login with your previous registration!
- 4. If you would like to make a reservation on behalf of someone else (e.g. your child), please let us know at the location provided.
- 5. Briefly describe your complaints!
- 6. Select the type of consultation: initial examination, control examination or prescription.
- 7. Click on the button to book your appointment. Thank you for choosing BMM!
If you are unable to make the appointment you have already booked, please, at least 24 hours before notify us of your intention to withdraw. This gives other patients the opportunity to get the medical care they need in time. Thank you for your cooperation and understanding!
Resignation: +36 1 44 33 433
If for the week of your choice cannot find an available appointment, for further assistance, please call our call-center at +36 1 44 33 433-phone number! Our staff will be happy to help you make an appointment with the doctor of your choice or another specialist according to your complaint.
Injury or anatomical predisposition?
Background to the development of patellar luxation can have several causes. One may be a direct trauma or an injury from a bad movement that has stretched or torn the internal stabilising ligaments of the knee.
However, in many cases anatomical conditions can also predispose to dislocation:
- shallower femoral trough (trochlear dysplasia),
- a higher kneecap,
- loose ligaments (hypermobility),
- X-leg deformity,
- Muscle disbalance in the anterior muscles of the thigh.
In these cases, even a slight strain or simple everyday movement can trigger a sprain. Medical examination and imaging tests (MR, X-rays) will help to determine whether the symptoms are caused by a simple injury or some other underlying factor.
Patellar instability:
when is physiotherapy enough and when is surgery an option?
Initially, many patients hope that stability can be restored without surgery - and in some cases it can. The type of treatment will always be determined by the severity and frequency of the dislocation, the patient's age, activity level and anatomy.
Conservative treatment options
After the first kneecap dislocation, if there has been no serious ligament damage or cartilage damage, usually conservative treatment is recommended by the orthopaedic specialist. The main elements are:
- Rest and pain relief - Relieving the load on the knee, icing it and, if necessary, anti-inflammatory drugs can help relieve the initial symptoms.
- Wearing a knee brace - A special brace to stabilise the patella prevents lateral displacement and supports ligament regeneration.
- Physical therapy - The key to treatment is targeted muscle strengthening, mainly by developing the inner thigh extensor muscle (VMO), which helps to keep the kneecap in the midline.
- Rehabilitation - In the later stages of therapy, it is also essential to improve coordination, balance and joint sensation (proprioception), especially in athletes.
The effectiveness of conservative treatment depends largely on the degree of patellar instability and the condition of the affected tissues. If the dislocation becomes recurrent or the kneecap continues to move unsteadily, a surgical solution may be justified, such as the MPFL plastics, which can provide long-term stability of the knee.

What is MPFL plasty and how does it help fix the knee cap?
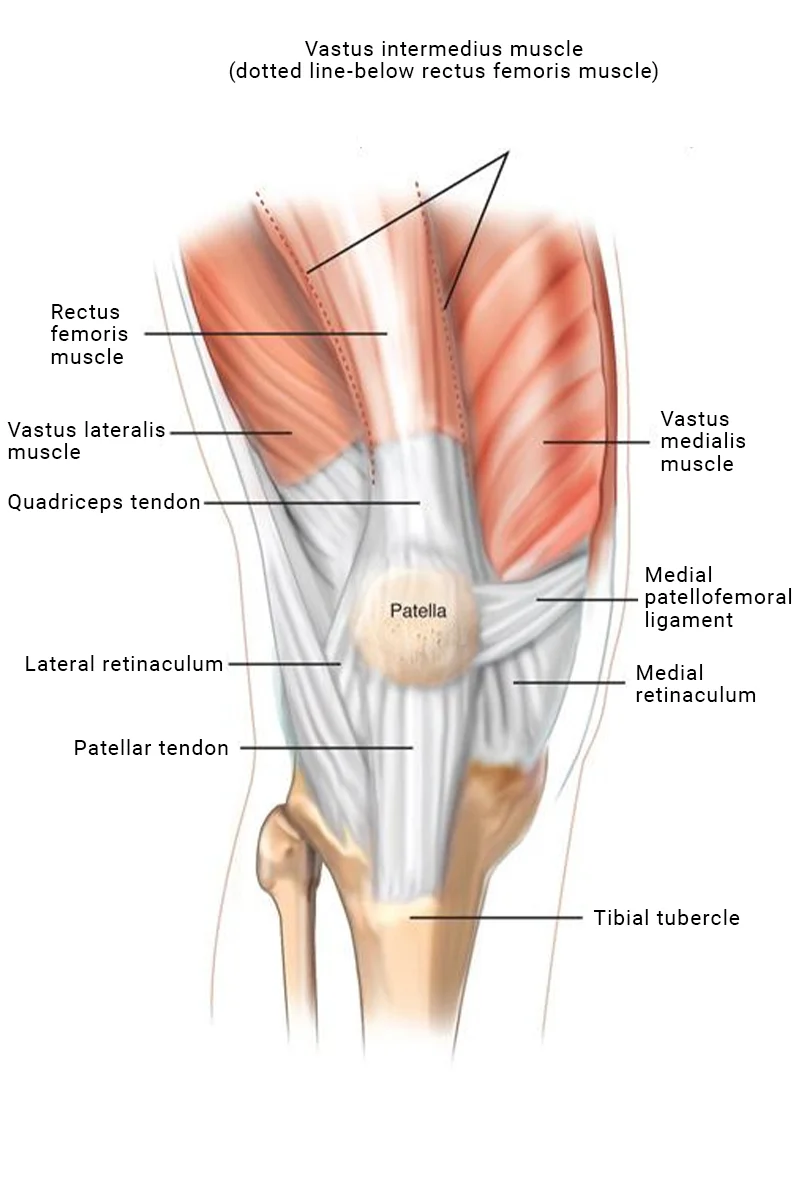
Several structures are responsible for the stability of the kneecap, including one of the most important is the medial collateral ligament, the MPFL (medial patellofemoral ligament). When this ligament is damaged, the kneecap can slip out of place more easily, especially when bending sideways.
The role of the MPFL ligament in knee function
The primary function of the MPFL ligament is to prevent lateral displacement of the kneecap during movement. In case of injury, recurrent dislocation is common, even if the external bony elements are intact. In such cases, muscle strengthening alone is not sufficient to provide stability.
How does MPFL plastic surgery work?
In MPFL surgery, the damaged ligament is replaced with a replacement made from the patient's own tendon, derived from the thigh muscle, and anatomically anchored in a precise location. The procedure small incisions, under general anaesthesia, and can usually be performed as part of a day case. The aim is to stabilise the kneecap's movement, preventing further dislocations.
Recovery after MPFL surgery: healing, rehabilitation and return to sport
In the post-operative period, the aim is to gradually restore muscle strength in the thigh and regain full range of motion in the knee joint. The recovery consists of several stages, which are always an individualised rehabilitation plan followed.

Post-operative care and pain relief
Following the procedure, the knee is protected with a special knee brace to ensure the correct position and range of motion is limited for healing. Postoperative pain is initially well controlled with medication. Already in the days following surgery passive movement can begin, to prevent joint stiffness.
Rehabilitation and return to sport
Physiotherapy is the key to recovery: the range of motion is gradually restored, followed by muscle strengthening. Restoring the symmetry of the muscles around the knee and improving the coordination of movement are of particular importance. The return to sport is gradual, usually 4-6 months after a period of time, depending on the stability of the knee and the patient's ability to bear the load.
MPFL plastics - frequently asked questions
The procedure usually takes 60-90 minutes and is performed under general anaesthesia.
The surgery involves several small incisions, so the scar is minimal, heals well and is aesthetically pleasing.
The MPFL surgery fee depends on several factors, so we can give you an exact amount after a personal consultation. Contact us with confidence To Dr. Péter Doszkocs, who will be happy to provide detailed information.
Yes, after proper rehabilitation, most patients can return to sport at full fitness, typically within 4-6 months.

Dr. Péter Doszkocs
Orthopaedic traumatologist, hip and knee surgeon, lower limb specialist, robotic surgeon
Don't put off treating kneecap problems - when can a knee specialist help?
If your kneecap has dislocated more than once or you feel unsteady when walking, running or playing sports, you should seek specialist help. Recurrent kneecap sprains are not only uncomfortable, but long-term cartilage damage and persistent pain can also lead to.
Dr. Péter Doszkocs orthopaedic-traumatologist senior physician is a renowned expert in the treatment of knee instability, who performs MPFL plastic surgery using modern, precise techniques.
Make an appointment with Dr. Peter Doszkocs and take the first step towards a more stable, safer knee!